How small medical practices can use data analytics and AI to improve patient outcomes, streamline operations, reduce billing errors, and stay HIPAA-compliant.
Small healthcare practices face tight budgets, limited teams, and complex regulations. But data analytics can help turn these challenges into opportunities. By analyzing data from EHRs, billing systems, and patient interactions, practices can improve patient care, reduce costs, and streamline operations. Here’s how:
Modern tools like AI-powered platforms and cloud-based SaaS solutions make analytics affordable and accessible for smaller practices. Start with clear goals, track metrics like readmission rates or claim denial rates, and ensure compliance with HIPAA and other regulations. With the right approach, data analytics can help small practices thrive.
To make the most of data analytics in healthcare, it's crucial to understand the basics: where your data originates, the different types of analytics available, and the rules that govern its use. These foundational elements are the building blocks for exploring operational and clinical analytics, which we’ll delve into later.
Small practices collect data from a variety of sources, each offering unique insights. The cornerstone is Electronic Health Records (EHRs), which store essential clinical information. This data can help monitor care quality, predict readmission risks, and tailor treatment plans to individual patients.
Practice management and scheduling systems are another key source, providing operational data like patient flow, provider schedules, and room usage. Analyzing this information can help optimize appointments, reduce no-shows, and align staffing with demand. Similarly, insurance claims and revenue cycle management (RCM) systems track billing, payer responses, and reimbursements. By examining this data, you can identify claim denials and improve financial performance.
Additionally, patient-generated data from wearables, mobile apps, and portals offers insights into lifestyle habits and behaviors, enabling proactive chronic disease management. Meanwhile, marketing and CRM data can help align advertising efforts with practice capacity, such as pausing campaigns for fully booked locations.
Many small practices struggle to fully utilize these data sources. For instance, only 57% of healthcare organizations leverage their data for informed decision-making, and 67% cite difficulties in data analysis as a major barrier to improving patient outcomes. Often, the issue lies in disconnected platforms that prevent clinical, operational, and financial teams from sharing information.
Once you’ve identified your data sources, the next step is to focus on metrics and analytics. Different types of analytics serve distinct purposes:
For small practices, key metrics include operational, financial, and clinical indicators. Operational metrics like average patient wait time, cancellation/no-show rate, and staff-to-patient ratio directly affect patient experience and care quality. Financial metrics such as claims denial rate (aim for below 5%), accounts receivable turnover, and average treatment charge are crucial for maintaining financial health. Clinical metrics include readmission rates, patient satisfaction scores, and medication error rates.
Using benchmarks that account for patient complexity ensures fair comparisons. For example, the average patient mortality rate across the industry is about 2%, and readmissions within 30 days cost the U.S. healthcare system over $50 billion annually.
While data analytics offers immense potential, compliance with regulatory standards is non-negotiable. Any use of patient data must align with federal and state laws. The HIPAA Privacy Rule protects "protected health information" (PHI) and applies to all healthcare providers transmitting electronic health data. The HIPAA Security Rule further mandates safeguards - administrative, physical, and technical - for securing electronic PHI (ePHI).
The HITECH Act reinforces HIPAA by imposing stricter penalties for violations, ranging from $141 to over $2 million per incident, depending on negligence levels. It also extends privacy and security requirements to business associates. Any third-party vendor handling PHI must sign a Business Associate Agreement (BAA).
"The Privacy Rule ensures secure patient data flow while protecting individual health information."
To minimize compliance risks, work with de-identified data whenever possible. De-identified data is exempt from HIPAA regulations and can be processed using either the "Expert Determination" method (statistical verification) or the "Safe Harbor" method (removal of 18 specific identifiers). Additionally, adhere to the minimum necessary standard, which limits PHI use to the smallest amount required for the task.
State-level laws may impose stricter rules than HIPAA. For example, the California Consumer Privacy Act (CCPA), Washington's My Health My Data Act (MHMDA), and Texas HB300 introduce additional requirements. Before adopting analytics tools, confirm that vendors will sign a BAA, have undergone third-party security certifications, and comply with both federal and state laws. Regular risk assessments, role-based access controls (RBAC), and data access audits are essential for maintaining compliance.
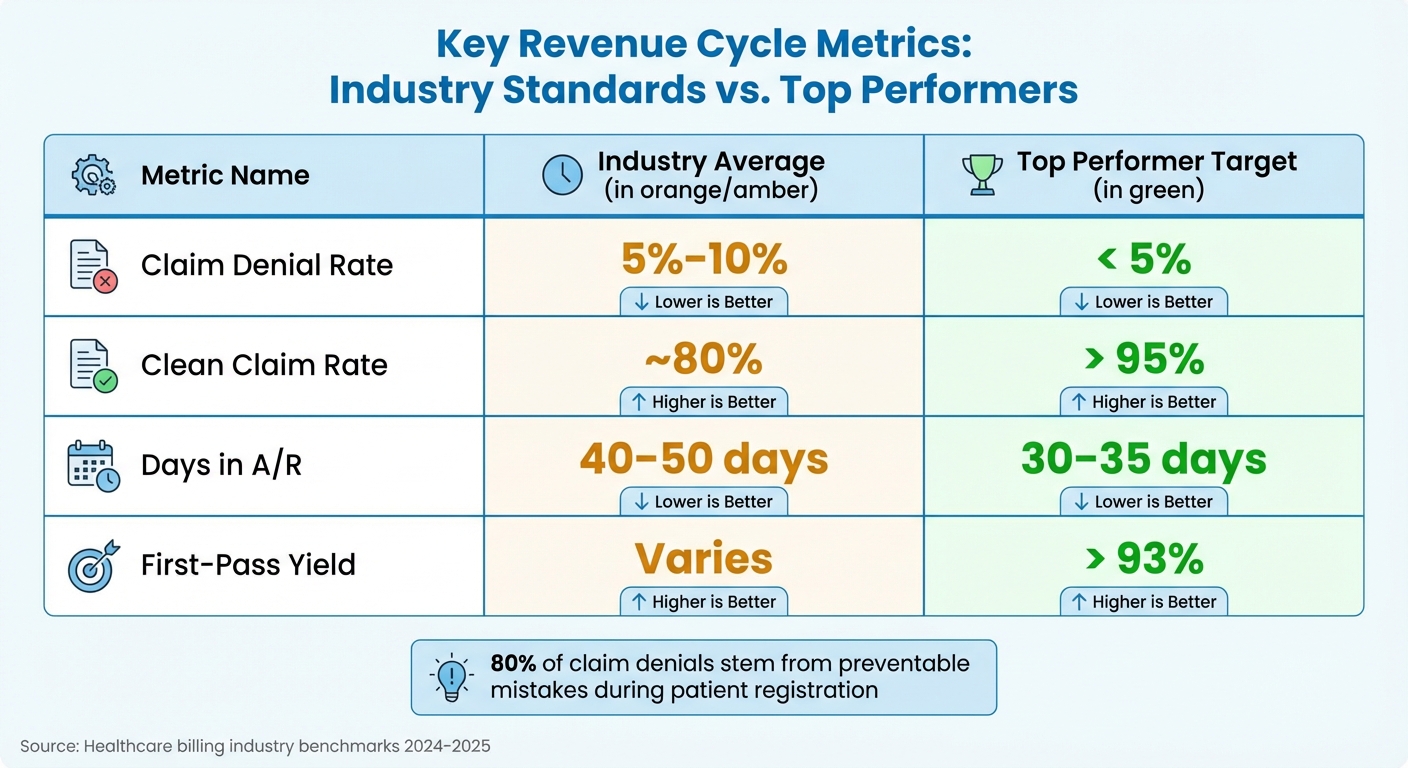
Key Healthcare Analytics Metrics: Industry Averages vs Top Performer Targets
Once you've tackled data sources and compliance, it's time to use analytics to smooth out workflow hiccups - like issues with data transfers between scheduling systems and patient records. These operational adjustments align with the broader objective of utilizing data analytics to enhance patient care and streamline practice efficiency.
The front office is the heartbeat of your practice. Any inefficiencies here affect everything else. Real-time dashboards showing patient status, room availability, and pending tasks give your team a shared view of operations. Instead of scrambling to fix problems after they cause delays, you can identify issues - like overbooked schedules or late arrivals - in real time and make immediate adjustments.
A major red flag is reliance on "human bridges", where staff manually re-enter data between disconnected systems. This indicates deeper workflow issues. Solutions like two-way, HIPAA-compliant texting can cut routine phone calls by half. Mobile-friendly intake forms that sync directly with your EHR eliminate check-in delays and reduce manual data entry.
"Bottlenecks don't disappear with more effort; they disappear when you fix the system." - Gregory Vic Dela Cruz, Curogram
Some practices are even using AI calling agents to handle appointment bookings, rescheduling, and cancellations, freeing up staff to focus on more complex tasks. The impact is clear: better flow coordination can reduce patient wait times by 15% to 30%, and AI-powered medical scribes have been shown to increase patient interaction time by 56%.
With a more efficient front office, you can turn your attention to improving billing and revenue processes.
Billing errors affect nearly 30% of patients and show up in 20% of claims, costing time, money, and trust. About 80% of claim denials stem from preventable mistakes during patient registration and insurance verification.
To stay on track, monitor these key metrics:
| Metric | Industry Average | Top Performer Target |
|---|---|---|
| Claim Denial Rate | 5%–10% | < 5% |
| Clean Claim Rate | ~80% | > 95% |
| Days in A/R | 40–50 days | 30–35 days |
| First-Pass Yield | Varies | > 93% |
Automated eligibility checks at every visit can prevent front-end denials. Standardized front-desk workflows, complete with checklists, ensure critical details like policy numbers and birth dates are accurate. Keeping "Charge Capture Lag Time" - the gap between service delivery and billing - under two days is key to maintaining steady cash flow.
For instance, in December 2025, Magnolia Family Urgent Care boosted its first-pass claims rate to 93%, up from below 50%, by adopting Practice EHR's AI Claim Editor. This tool proactively flagged coding errors and missing modifiers before submission, slashing denial rates and reducing manual fixes. Integrated analytics dashboards further helped decrease claim write-offs by 29% and improved clean-claim rates by 19%.
Another game-changer? Text-to-pay systems. Sending secure payment links via SMS not only speeds up cash flow but also simplifies the patient payment experience, cutting down on back-and-forth phone collections.
Strengthening revenue processes lays the groundwork for broader efficiency gains through automation.
Manual processes don't just slow things down - they invite mistakes. Automated workflows can cut claims-handling times by 50% to 70% compared to manual methods. Modern platforms leverage AI and natural language processing (NLP) to extract coding justifications, predict denials, and automate insurance eligibility checks.
Take MedOps, for example. This platform uses AI for real-time insurance verification, catching errors early and integrating seamlessly with existing systems. By addressing issues before they escalate to billing or claims, MedOps helps practices maintain high clean-claim rates and faster reimbursements. These automated workflows reduce administrative burdens while improving both operational and clinical efficiency.
Switching from batch processing - letting tasks pile up - to "Just-In-Time" processing, where tasks are completed as they come in, prevents administrative bottlenecks. Instead of trying to improve everything at once, focus on the single resource that's slowing you down. Whether it's a scheduling issue, billing delay, or staffing gap, analytics can pinpoint the constraint so you can tackle it directly, as outlined in the Theory of Constraints.
This targeted approach ensures that your practice runs smoothly and efficiently.
While operational efficiency is crucial, the real game-changer is how clinical analytics can help prevent crises altogether. By shifting from reactive care - addressing issues as they arise - to proactive care, healthcare providers can intervene early, reducing emergency room visits and hospital stays. This proactive approach aligns seamlessly with the operational improvements discussed earlier.
A good starting point is tracking key patient outcome metrics like mortality rates, 30-day readmission rates, and average length of stay (ALOS). For chronic conditions, it’s also essential to monitor how well patients are managing diseases like hypertension or diabetes and whether they’re completing preventive care screenings.
Consider this: a 2014 study led by Dr. Christine Pitocco from Stony Brook University revealed that only 20.8% of hospitals were performing at their peak quality levels. The study estimated that if all hospitals achieved 100% performance, they could have prevented 11,722 deaths and 17,840 readmissions while reducing the average length of stay by 0.71 days.
To improve outcomes, focus on metrics that directly influence patient care. Start with descriptive analytics to review historical trends, then dive into diagnostic analytics to uncover the reasons behind specific patterns - like why certain patient groups experience higher readmission rates.
"Every number is a person." - Stephanie Jackson, MD, Senior Vice President and Chief Clinical Officer, HonorHealth
These metrics are the foundation for identifying high-risk patients and prioritizing their care effectively.
Once you’ve gathered insights from quality metrics, the next step is risk stratification. This process uses analytics to identify patients most likely to face complications or require hospitalization, enabling healthcare teams to focus resources where they’ll make the biggest difference.
Dr. Amanda Williams, a physician with Physicians Group of Southeastern Ohio, shared her experience:
"I'm part of a small practice that previously lacked advanced analytics; partnering with a larger platform allowed us to implement risk models we couldn't build in-house".
The impact was immediate:
"It's amazing because I can identify a high-risk patient, and then I know if they're high-risk that we need to increase their PCP touchpoints to make sure that we keep them out of the ER and out of the hospital and essentially wrap our chronic care management team around those patients".
By integrating data from electronic health records (EHRs), pharmacy claims, and social determinants of health (SDOH) - like poverty levels or local air quality - accuracy improves significantly. Deep learning models analyzing EHR data have even outperformed traditional clinical scoring systems in predicting outcomes like mortality, readmission risk, and length of stay.
Building on risk stratification, predictive analytics takes things a step further by forecasting future events. These models can anticipate specific scenarios, such as patients likely to miss appointments or whose chronic conditions may worsen. With this foresight, healthcare teams can act early, whether through outreach or adjusted treatment plans.
For instance, incorporating medication adherence metrics improved predictions of cardiovascular events in diabetic patients by 18%. Similarly, practices that adopted predictive analytics for readmission risk saw their 30-day readmission rates drop by 12%.
The good news? You don’t need an in-house data science team to get started. Many platforms now offer "analytics-as-a-service", providing ready-to-use predictive models that integrate seamlessly with EHR systems. Just make sure the platform you choose accounts for SDOH factors and complies with HIPAA standards, including encryption and Business Associate Agreements (BAAs).
Start small. Focus on straightforward use cases like predicting no-shows or identifying overdue screenings. Over time, expand to more complex models, such as forecasting which patients with hypertension might develop heart failure or depression. With these insights, you can move from simply reacting to crises to actively preventing them.
To make the most of analytics for improving patient care and streamlining operations, selecting the right tools and adopting effective strategies is key. Fortunately, small practices don’t need enormous budgets or IT departments to get started. Cloud-based platforms eliminate the need for physical servers, and many solutions are designed with smaller practices in mind.
Before purchasing new software, take a closer look at your EHR's built-in reporting features. Many EHRs already include dashboards that track metrics like billing, no-show rates, and revenue per visit.
If your practice is ready to go beyond basic reporting, there are cost-effective options available. Tools like Power BI, priced at $10 per user per month, SimplePractice at $29 per month, and MDToolbox at $28 per month, offer integrated analytics capabilities. AI-powered tools are also becoming more accessible. For example, Freed and similar AI scribes can save providers about 63 seconds per chart, helping to reduce documentation fatigue. For practices that want to create custom dashboards without hiring developers, platforms like UI Bakery offer free plans and pro options starting at $5 per user per month. According to a 2023 AMA survey, 71% of small-clinic doctors expressed a desire for software requiring fewer clicks and offering better layouts to combat burnout.
When choosing tools, involve your team to ensure the new system fits seamlessly into your workflow and enhances overall efficiency. Always request task-specific demos - ask vendors to demonstrate how their system handles specific needs like triage, referrals, or identifying missed appointments. Pay attention to hidden costs such as data migration fees, e-prescribing charges, or third-party integration expenses. If your practice involves home visits or bedside care, prioritize tools with strong mobile functionality and voice-to-text features.
"The right EMR boosts claim approval by 5% or more. For a three-doctor office, that means thousands more in revenue." – HelpSquad
For more comprehensive solutions, MedOps offers AI-powered insurance verification and workflow automation tailored for small healthcare practices. This platform integrates with existing systems to streamline processes, reduce errors, and improve staff efficiency.
Once you’ve chosen the right tools, the next step is to define and track meaningful metrics.
After selecting your tools, focus on metrics that matter. Use the SMART framework - Specific, Measurable, Achievable, Relevant, and Time-bound - to set realistic goals based on your practice’s historical data and industry standards. Start small by monitoring one or two impactful KPIs, such as no-show rates or days in accounts receivable.
Balance your KPIs across four main areas:
High-performing practices often achieve a clean claim rate of 95% or higher and a first-pass resolution rate above 90%. Extract data from your EHR, practice management system, and billing software, then visualize it using real-time dashboards. Regularly review your KPI data - monthly or quarterly - to catch and address negative trends early. To ensure consistency, make sure all staff agree on definitions (e.g., distinguishing between a "no-show" and a "cancellation").
"IMS is very modern - sophisticated - it works seamlessly, and it's enabled us to probably cut our billing time in half." – Marilyn Benck, Table Mountain Rancheria Medical Center
For successful implementation, seamless integration of your data systems is essential. Start by documenting all your data sources, such as EHRs, lab systems, insurance platforms, and patient portals. Use FHIR-enabled APIs, which allow systems to communicate without requiring custom coding. Nearly 90% of health systems have adopted FHIR (Fast Healthcare Interoperability Resources).
If you're working with older systems, middleware tools like Mirth Connect can help bridge the gap to modern analytics platforms. These solutions resolve data silos and provide real-time access to fragmented patient information. To protect sensitive data, ensure all integrations use end-to-end encryption and comply with HIPAA and HITECH regulations. With 67% of healthcare organizations experiencing ransomware attacks in 2024, prioritizing security is non-negotiable.
Establishing clear data governance is equally important. Define who owns the data, assign stewardship roles, and implement role-based access controls to maintain data integrity. Set up automated validation processes to eliminate duplicate records and inconsistent formats before data enters your analytics system. Poor integration practices can lead to duplicate or irrelevant data - issues reported by 60% of health systems.
Start with a high-impact project, such as reducing claim denials or improving patient throughput. Involve clinical leads early to ensure the tools align with actual workflows, not just IT preferences. Train your team on FHIR standards and new workflows to maximize the tools’ effectiveness. Regular audits, both manual and automated, are necessary to meet compliance and security standards.
"Governance shouldn't be a barrier to using data. It should be the reason your teams trust the data." – Analytics8
The healthcare sector generates 30% of the world’s data each year, with annual growth at 48%. By selecting the right tools and focusing on effective implementation, small practices can harness this wealth of information to stay competitive while continuing to provide personalized care.
Small practices don’t need massive budgets or advanced IT infrastructures to harness the power of data analytics. The secret lies in starting small and focusing on targeted, impactful projects that build momentum and confidence over time. By steering clear of high-risk, large-scale initiatives, practices can adopt a step-by-step approach that delivers quick wins and measurable results.
Creating a culture where decisions are guided by actionable insights is crucial. Begin by cleaning and standardizing your existing data - this is essential since analysts often spend up to 80% of their time just preparing data for analysis. From there, set one or two specific, measurable goals, such as lowering hospital readmission rates, and track progress using the SMART framework. These foundational steps pave the way for achieving meaningful financial and operational improvements.
The potential financial benefits are immense. AI-driven predictive analytics could save up to $360 billion annually in the United States alone, while the healthcare analytics market is expected to grow to $167 billion by 2030, with an annual growth rate of 21.1%. For small practices, this means opportunities to cut costs through automated administrative tasks and streamlined operations.
"Small data will tell us more than all of the big data we have now." – Abbas Mooraj, Vice President, Optum
MedOps is designed to help small practices take advantage of these opportunities with AI-powered tools like insurance verification and custom workflow automation. Its seamless integration with existing systems ensures real-time validation, minimizing errors and freeing up staff to focus on what matters most - patient care. With healthcare data expanding at a rate of 36% annually, the moment to act is now. Start with a pilot project, evaluate the results, and scale what works. This practical, data-driven approach ensures your practice can evolve sustainably and deliver better care for your patients. Your data holds the key to transformation.
To get started with data analytics, take a close look at your current data systems and pinpoint key performance indicators (KPIs) that match your practice's objectives. Begin with budget-friendly, cloud-based tools that are simple to set up and can seamlessly work with your existing systems. Prioritize keeping your data accurate and well-structured.
You might want to try a pilot project to explore the benefits of analytics in a specific area, such as streamlining appointment scheduling or monitoring patient outcomes. Make sure your team is equipped to understand and use data effectively - this might involve training or even partnering with analytics experts. Above all, aim to build a data-driven mindset within your team by encouraging decisions based on insights rather than guesswork.
To deliver better care and improve patient outcomes, small healthcare practices should prioritize tracking a handful of key metrics that offer meaningful insights into care quality and efficiency. These metrics include:
By zeroing in on these areas, small practices can make informed, data-driven decisions to improve both the quality of care and the efficiency of their operations, ultimately supporting healthier outcomes for their patients.
Small healthcare practices can maintain compliance with data privacy regulations by focusing on a few essential practices. First, always ensure informed consent by clearly explaining to patients how their data will be collected, used, and stored. Transparency builds trust and aligns with legal requirements.
It's also critical to establish strong security measures across all systems to safeguard sensitive patient information. Providing patients with clear options to access, manage, and control their data further reinforces privacy rights and compliance efforts.
Conducting regular privacy impact assessments can help identify potential vulnerabilities and address them proactively. And, of course, compliance with key regulations like HIPAA and CCPA is non-negotiable for healthcare providers operating in the U.S. Following these rules not only ensures legal adherence but also strengthens patient trust.