How clearinghouses streamline clinic billing: reduce errors, speed reimbursements, automate claim scrubbing, and improve cash flow with secure EDI and AI checks.
Handling medical claims can feel overwhelming, but medical claims clearinghouses simplify the process. These third-party services act as intermediaries between clinics and insurance companies, ensuring claims are accurate, properly formatted, and securely transmitted. Here’s why they matter:
How Medical Claims Clearinghouses Process Healthcare Claims
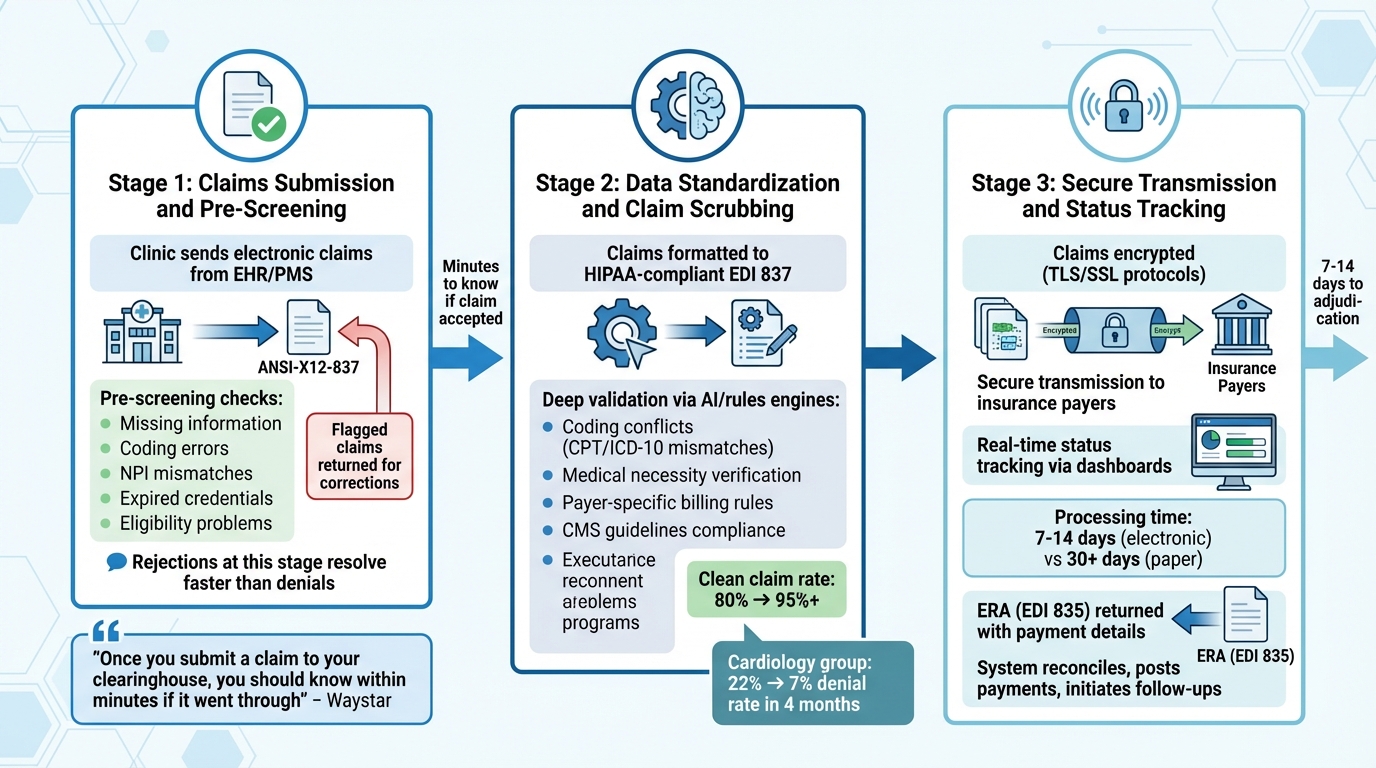
Grasping the clearinghouse workflow is key for clinics to understand how claims progress from submission to payment. The system is built to catch errors early, ensure data consistency, and maintain security while offering transparency at every stage.
Your clinic sends electronic claims directly from its EHR or PMS. These claims include patient details, ICD-10 codes, CPT/HCPCS codes, insurance information, and your NPI number. Most claims are submitted in the ANSI-X12-837 file format.
Once received, the clearinghouse pre-screens each claim for potential issues, such as missing information, coding errors, NPI mismatches, expired credentials, or eligibility problems. Claims that don’t pass these checks are flagged and sent back for corrections before they ever reach the insurance payer. This step is crucial because rejections at the clearinghouse level are quicker to resolve compared to denials, which occur after the payer processes the claim and take longer to address.
After pre-screening, claims move on to standardization and more detailed error checks.
Claims that pass the initial screening are formatted into a standardized, HIPAA-compliant EDI 837 format. This ensures compatibility across different payer systems.
Next, the claims undergo a deeper validation process known as claim scrubbing. Using advanced rules engines or AI technology, the clearinghouse checks for coding conflicts (like mismatched CPT and ICD-10 codes), verifies medical necessity, and ensures compliance with payer-specific billing rules and CMS guidelines. For instance, in April 2025, a cardiology group reduced its denial rate from 22% to 7% in just four months by using AI-powered claim scrubbing to catch missing authorizations before submission. By improving claim accuracy, scrubbing can push the clean claim rate from an average of 80% to 95% or higher, speeding up the reimbursement process.
After scrubbing and validation, claims are encrypted using TLS/SSL protocols to ensure HIPAA compliance and protect patient data during transmission. The clearinghouse then securely sends the claims to the appropriate insurance payers.
"Once you submit a claim to your clearinghouse, you should know within minutes if it went through or if it needs to be corrected and resubmitted." – Waystar
Modern clearinghouses also offer real-time status updates through dashboards or EHR integrations. These tools let you monitor live claim statuses, track the percentage of pending or denied claims, and receive instant alerts for flagged claims. Electronic claims are typically adjudicated within 7–14 days, compared to over 30 days for paper claims. Once processed, the payer sends back an Electronic Remittance Advice (ERA) in EDI 835 format, detailing payments, adjustments, or denial reasons. Your billing system then reconciles the ERA, posts payments, and initiates follow-ups for any unpaid or denied claims.
Medical claims clearinghouses play a crucial role in improving clinic operations. By catching errors early, speeding up payment processes, and automating repetitive tasks, they help clinics save time and focus more on patient care. Let’s break down the key advantages.
One standout feature of clearinghouses is their ability to dramatically reduce errors through claim scrubbing. While manual claims can have error rates as high as 28%, electronic submissions cut this down to just 2–3%, resulting in 25% fewer errors overall.
The scrubbing process flags common issues like invalid CPT or ICD-10 codes, missing modifiers, incorrect patient information, and incomplete demographics. With automated edits, claim rejections can drop by 20–30%. Maintaining a high first-pass rate - ideally 95% or higher - ensures fewer delays and boosts cash flow by reducing the need for rework.
Lower error rates naturally translate into faster payments. Clearinghouses can improve reimbursement speeds by up to 30%. Additionally, features like real-time tracking give clinics the ability to monitor claim statuses, quickly address issues, and maintain a clear view of their revenue pipeline.
Detailed Electronic Remittance Advice (ERA) makes it easier to resolve denials quickly, helping accelerate the revenue cycle. Clinics that adopt systematic benchmarking with clearinghouse services often see operating margins up to 18% higher than those that don't benchmark.
Automation significantly reduces the time spent on manual tasks. For example, processing a claim manually takes about 8.5 minutes, but clearinghouses can handle it in seconds. This efficiency can cut administrative costs by as much as 30%.
Batch processing allows clinics to submit multiple claims at once, and standardized formatting simplifies interactions with payers. Modern clearinghouses also offer real-time revenue cycle management dashboards, providing granular analytics like denial trends by payer and claim aging. These tools help clinics address stalled claims more quickly. By streamlining these processes, staff can shift their focus from paperwork to delivering better patient care.
Picking the right clearinghouse is a crucial step in managing your clinic's revenue cycle effectively. With nearly 26% of medical claims being rejected or denied on the first submission and up to 40% of denied claims never being followed up on, the stakes are high. The wrong choice can lead to delayed payments, disrupt workflows, frustrate your staff, and harm your clinic's financial health. To make the best decision, focus on these key factors to ensure the clearinghouse aligns with your clinic's specific needs.
First, confirm that the clearinghouse adheres to strict HIPAA compliance and security protocols. Patient data must be safeguarded through strong encryption, access controls, and reliable disaster recovery plans. Beyond security, ensure the clearinghouse connects seamlessly with all your regular payers and supports your specific claims mix, whether that involves outpatient, dental, or Medicaid submissions. A 2021 KFF study found that 18% of in-network claims were denied for excluded services, while 9% were denied due to missing prior authorization. Payer-specific validation is, therefore, a must-have feature.
Integration with your clinic's existing systems is equally important. The clearinghouse should work effortlessly with your electronic health record (EHR) and practice management systems. Look for options with native integrations or API-based connectivity that support standards like HL7 and FHIR, ensuring smooth, automated data exchange. If your EHR vendor recommends specific clearinghouses, this can simplify the process and save you from needing custom interfaces. Always test sample claims during a trial period to verify accurate data transmission and ensure your workflows remain efficient.
User experience is another critical factor. Your staff should have access to an intuitive dashboard that provides clear error reports, real-time claim status updates, and accessible communication channels for problem-solving. Responsive, in-house customer support is essential for quickly addressing claim disputes and troubleshooting issues.
Many modern clearinghouses now use AI-powered tools to minimize errors before claims are submitted. These tools analyze large datasets to predict outcomes, identify patterns, and flag issues like invalid codes, missing modifiers, or payer-specific requirements. Real-time claim edits powered by AI can reduce denials by 30–50%, while automated claim scrubbing ensures compliance with payer guidelines and CMS regulations.
For example, MedOps provides AI-driven validation, custom workflow automation, and seamless integration to help clinics reduce errors and improve efficiency. These tools can optimize claim validation, maintain high first-pass acceptance rates, and speed up reimbursements.
Additionally, clearinghouses offering actionable claim status summaries make it easier for staff to prioritize payments, avoiding duplicate efforts. Automated payment posting using Electronic Remittance Advice (ERA) further simplifies the reconciliation process, saving time and effort.
Understanding the pricing model is essential before committing to a clearinghouse. Some charge a fixed monthly fee, while others use pricing based on claim volume. Additional services like eligibility checks, claim status updates, and remittance receipts are often billed separately, so be sure to account for these costs. Request clear, transparent pricing to avoid surprises, and weigh the overall savings from reduced denials and improved efficiency when evaluating options.
Scalability is another important consideration. Choose a clearinghouse that can handle growing claim volumes, support additional payers, and adapt to new regulations without requiring a complete system overhaul. Avoid long-term contracts with unclear termination policies. Before diving into options, take the time to assess your clinic’s daily workflows, common bottlenecks, claim volume, specialty requirements, and payer mix. This will help you identify the features you truly need, rather than opting for a solution with unnecessary extras that could complicate your administrative processes.
Medical claims clearinghouses play a crucial role in helping clinics simplify their revenue cycle and lighten administrative workloads. By automating processes like claim scrubbing, standardizing data formats, and catching errors before submission, they help reduce denial rates and speed up reimbursements. The result? Quicker payments, better cash flow, and fewer headaches from rework.
But the benefits don’t stop there. Clearinghouses take on the tedious task of data entry, freeing up your team to focus on what matters most - patient care. They also manage the technical side of things, like converting billing data into standard electronic formats, ensuring HIPAA compliance, and securely transmitting information to various payers.
Today’s clearinghouses go even further by utilizing real-time validation and payer-specific, AI-driven checks. These tools help cut down on denials and improve overall efficiency.
To make the most of these advantages, choosing the right clearinghouse is key. Consider your clinic's unique needs, such as payer mix, claim volume, integration requirements, and budget. Tools like MedOps offer features like AI-powered validation, workflow automation, and seamless integration to reduce errors and boost productivity. Before committing, take time to evaluate your current workflows and test sample claims during a trial period to ensure the platform supports your clinic’s long-term goals.
Medical claims clearinghouses are essential in reducing errors by automatically reviewing claims for issues such as missing details, incorrect codes, or formatting problems before submission to insurance providers. This process, known as claim scrubbing, catches and corrects errors upfront, significantly lowering the chances of claim rejections or denials.
By making sure claims are accurate and complete, clearinghouses help clinics save valuable time and resources. This streamlining of the claims process allows healthcare providers to shift their focus from administrative tasks to what matters most - delivering quality patient care.
When selecting a medical claims clearinghouse, it's essential to consider factors like user-friendliness, dependability, and how well it integrates with your current systems. A good clearinghouse should offer real-time claim status updates and provide detailed error reports to help you quickly spot and fix problems.
Make sure the clearinghouse prioritizes patient data accuracy and security while also providing responsive customer service. It's equally crucial to confirm that they have experience working with your type of practice and are familiar with the specific requirements of your payers to help prevent processing delays.
AI-driven tools integrated into clearinghouses play a crucial role in reducing claim denials by spotting and fixing errors in claims before submission. These tools work in real time to check the accuracy of patient details and billing information while ensuring claims meet insurance payer guidelines.
By addressing issues like missing details or incorrect codes upfront, AI helps lower the chances of claim rejections. This not only speeds up the reimbursement process but also saves clinics valuable time, cuts down on delays, and streamlines the overall claims management workflow.